The Biomechanics of the
Spine in the Treatment of
Spine Pain Syndromes
The Management of Spine
Pain Syndromes Through the
Understanding and Treatment of the
Spine as a Single Functioning Unit
It is convenient to divide and discuss the human spinal column into four regions:
- Cervical spine (neck)
- Thoracic spine (middle back)
- Lumbar spine (low back)
- Pelvis (the base of the spinal column)
Although this classification is convenient, it is also misleading and occasionally harmful. The discussion presented here reminds us that the four convenient regions of the spinal column are interrelated both biomechanically and neurologically. In short, the entire spinal column is a single functioning unit.
Biomechanics
Ninety-three percent of chiropractic patients seek care for low back (63%) and/or neck pain (30%) (1).
The most common tissue source of chronic low back pain is the intervertebral disc (2). The most common tissue source for chronic neck pain is the facet joint capsules (3).
Human bipedal upright posture is a three-dimensional first class mechanical lever system (4, 5):
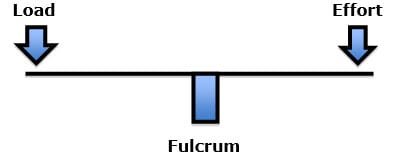
In the first class lever mechanical system, the fulcrum is located between the load and the effort. In human posture, the load is the weight multiplied by the distance away from the fulcrum. The effort to maintain a balanced structure is supplied by the muscles. All postural imbalances increase the load on the fulcrum and require muscle effort to prevent tipping over.
The fulcrum is the structure that bears the greatest mechanical stress. The fulcrum is the “weakest link” for mechanical degradation. Overly large loads with equalizing counterbalancing efforts will cause the structure to break at the fulcrum. An example would be using one’s hands to break a stick on one’s knee.
In the spine, the fulcrum of the first class lever of upright posture is primarily the vertebral body/disc, and the two facet joints. When the first class lever of upright posture is altered, for any reason, there is an increased mechanical load on the fulcrum, i.e. the spinal intervertebral discs and facet joints. Such increased mechanical loads accelerate degenerative joint disease and inflammation, altering the pain thresholds (4, 5, 6).
Postural distortions that cause spinal fulcrum stress may begin at the head. Or, postural distortions may also begin at the base of the spine, the pelvis. Pelvic leveling problems may be attributed to problems in the pelvis, but also in the feet, knees, hips, etc. The notorious “Leaning Tower of Pisa” is an example of a mechanical problem caused by an unleveled base.
The bottom line is that the primary tissues responsible for spinal pain (the disc and the facet) are the same tissues that function as the fulcrum of the first-class level of upright posture.
•••••
In the reference text The Spine, chapter 2 is titled (7):
“Applied Anatomy of the Spine”
This chapter is written by Wesley Parke, PhD. At the time of publication, Dr. Parke was Professor and Chairman, Department of Anatomy, University of South Dakota School of Medicine. In this chapter, Dr. Parke writes:
“Although the 23 or 24 individual motor segments must be considered in relation to the spinal column as a whole, no congenital or acquired disorder of a single major component of a unit can exist without affecting first the functions of the other components of the same unit and then the functions of other levels of the spine.”
The reference text Disorders of the Cervical Spine is written by rheumatologist John Bland, MD. Dr. Bland is a Professor of Medicine at the University of Vermont College of Medicine. Dr. Bland writes (8, 9):
“We tend to divide the examination of the spine into regions: cervical, thoracic, and lumbar spine clinical studies.
This is a mistake.
The three units are closely interrelated structurally and functionally – a whole person with a whole spine.
The cervical spine may be symptomatic because of a thoracic or lumbar spine abnormality, and vice versa!
Sometimes treating a lumbar spine will relieve a cervical spine syndrome, or proper management of the cervical spine will relieve low backache.”
For these biomechanical reasons, chiropractors often evaluate and treat regions of the spine that are asymptomatic yet functionally related to the region of primary complaint. As an example, improving the postural alignment of the head will reduce fulcrum spinal stress in the low back, reducing low back pain.
Neurology
By now (2019), nearly everyone is aware of the narcotic epidemic in the United States. Narcotics are pain drugs. Narcotics include both opiates and opioids (10):
Opiates are compounds that are purified directly from the opium poppy plant.
Opioids are a synthetic form of opium, made in a chemistry lab, like Fentanyl.
Both opiates and opioids suppress pain by attaching to receptors. Sadly, opiate receptors adapt quickly to these narcotic drugs and the pain suppression benefits are soon lost. Compensation for this receptor adaptation is increasing the dose or adding a second narcotic product. More sadly, increasing narcotic dose has numerous side effects, including addiction, mood changes, drowsiness, mental clouding, nausea, vomiting, constipation, and even death (11). A study published in the journal Pain Therapy in 2018 from Harvard Medical School states (12):
“Tragically, opioids claimed over 64,000 lives just last year [2017].”
Perhaps even more concerning is that 80% of heroin addicts in the United Stated begin their addiction with a narcotic prescribed for pain (13).
•••••
The understanding and management of chronic pain was significantly advanced in 1973 when Candace Pert (d. 2013) discovered the opiate receptor (14). Dr. Pert was an American neuroscientist and pharmacologist who was awarded a Ph.D. the following year (1974), from Johns Hopkins University School of Medicine.
By 1977, researchers determined that the opiate receptors in the upper brain stem (mesencephalon) were responsible for controlling pain throughout the body (15). The specific location for these opiate receptors was the grey matter surrounding the cerebral aqueduct, known as periaqueductal gray matter. The authors inserted electrodes (an invasive and risky endeavor) into the periaqueductal gray matter of the mesencephalon of six cancer patients suffering from intractable pain. They state (15):
“Relief of intractable pain was produced in six human patients by stimulation of electrodes permanently implanted in the periventricular and periaqueductal gray matter.”
In his 1979 book, The Brain, The Last Frontier, Richard Restak, MD, reviews this research, stating (16):
“Within the periaqueductal gray, a deep-seated brainstem area lying along the floor of the third ventricle, neurosurgeons at the University of California in San Francisco placed indwelling stimulating electrodes for pain relief in six patients afflicted with chronic, unremitting pain. Whenever the patients began to experience pain, they were able to shut it off via the activation of a battery-operated stimulator about the size of a pack of cigarettes. After activating the stimulator, all six patients—in accordance with earlier findings in other pain patients—experienced dramatic, long-lasting, and repeatable pain relief.”
“In order to test the hypothesis that pain relief was genuine and not just an example of a ‘placebo response,’ one patient was outfitted with a stimulator containing a ‘dead’ battery. The patient, a fifty-one-year-old woman with severe back and leg pain caused by cancer of the colon, anxiously reported that her pain had returned and the stimulator ‘wasn’t working.’ Replacement of a new battery led to immediate pain relief.”
Periaqueductal gray matter stimulation for pain control initiates what is know as activation of the Descending Pain Inhibitory Control System, and it has continued to receive reference text support ever since (17, 18, 19, 20). These studies indicate the following:
- Opiate receptors, when activated, inhibit pain.
- The periaqueductal gray matter of the mesencephalon is densely populated with opiate receptors.
- Electrical stimulation of the periaqueductal gray matter opiate receptors causes quick and complete pain relief throughout the body.
However, electrical stimulation of the periaqueductal gray matter opiate receptors for pain suppression is quite invasive and has logistical risks. Consequently, narcotic drugs, as noted above, have become increasingly used for pain control since the 1980s (21, 22). This approach to pain control has resulted in a national nightmare, well described in the political magazine Time that states (23):
“They’re the most powerful painkillers ever invented. And they’re creating the worst addiction crisis America has ever seen.”
“...9.4 million Americans take opioids for long-term pain.”
“Doctors so frequently prescribe the drugs known as opioids for chronic pain from conditions like arthritis, migraines and lower back injuries that there are enough pills prescribed every year to keep every American adult medicated around the clock for a month.”
“Now 4 of 5 [80%] heroin addicts say they came to the drug from prescription painkillers.”
“The American Academy of Neurology last year concluded that the risks of long-term opioid treatment for headaches and chronic low-back pain likely outweigh the benefits.”
Spinal Manipulation Science for Pain Evolves
Over the past century, chiropractors have observed that spinal manipulation in one region of the body would often alleviate pain in a different, untreated region of the body. Consequently, chiropractors adjust (specific manipulation) all documented biomechanical lesions, regardless of the patient’s pain presentation.
In addition to these biomechanical considerations, published studies show a neurological explanation for the effect of spinal adjusting in the relief of pain in non-treated body areas. Interestingly, these explanations involve the activation of the periaqueductal gray matter descending pain inhibitory control system.
In 1996, a study was published in the journal Pain, titled (24):
The Initial Effects of a Cervical Spine Manipulative
Physiotherapy Treatment on the Pain and
Dysfunction of Lateral Epicondylalgia
Importantly, these authors were treating elbow pain in patients, who were not suffering from radiculopathy or referred pain, without touching or treating the offending elbow. In contrast, treatment was directed towards the dysfunctional joints of the patient’s cervical spine. The most commonly found biomechanical dysfunction was hypomobility of the joints of the lower cervical spine. The authors made the following comments:
“This study has demonstrated a clear hypoalgesic effect of a manipulative therapy technique [applied to the cervical spine] in the period immediately following its application in a group of patients with lateral epicondylalgia.”
“A significant treatment effect beyond placebo or control was demonstrated.”
“The beneficial effects of treatment [cervical manipulation] may continue after its application.”
The author’s theoretical model to explain their results involved manipulative therapy activation of the hypoalgesic effects of the endogenous supraspinal pain inhibitory systems.
“The [manipulative] treatment technique used in this study provided a non-noxious sensory input at the cervical spine which resulted in a reduction of elbow pain that outlasted the duration of its application.” “This is thought to activate the descending pain inhibitory system as a major component of their pain-relieving effects.”
The descending pain inhibitory system is activated by stimulation of the periaqueductal gray (PAG).
“These findings indicate that manipulative therapy may constitute an adequate physical stimulus for activating the descending pain inhibitory system.”
“Manipulative therapy [may] recruit the descending pain inhibitory system, through which it exerts a portion or all of its pain-relieving effects. That is, manipulative therapy applied to the cervical spine produces a sensory input which could be sufficient to activate descending pain inhibitory system.”
“In a group of patients with lateral epicondylalgia, a manipulative therapy treatment technique applied to the lower cervical spine produced hypoalgesia at the elbow as manifest by increased pressure pain threshold, increased grip strength, improved neurodynamics and reduced pain over a 24 h period. This finding substantiates clinical observations that manipulative therapy is capable of producing improvements in pain and function immediately following application.”
Another study indicating that spinal manipulation is capable of activating the descending pain control system was published in the Journal of Back Musculoskeletal Rehabilitation in 2014, and titled (25):
The role of the Descending Inhibitory Pain Mechanism
in Musculoskeletal Pain Following High-Velocity,
Low Amplitude Thrust Manipulation: A Review of the Literature
The objective of this review was to investigate the role of the Descending Inhibitory Pain Mechanism in musculoskeletal pain following high-velocity, low amplitude thrust manipulation, as well as to identify the pain-relieving importance of this technique within clinical practice. The authors of this article make the following comments and conclusions:
“Although the antinociceptive effect of high-velocity, low amplitude thrust manipulation has been recognized by numerous systematic reviews, the underlying mechanism for manipulation-related pain relief remains poorly understood. An increasing number of studies have explored its analgesic mechanism suggesting that the excitation of the descending inhibitory pain mechanism might play the most important role for musculoskeletal pain relief.”
“Findings from current literature support that high-velocity, low amplitude thrust manipulation has a profound influence on nociceptive stimulus via the possible activation of the descending inhibitory pain mechanism. It seems that the application of this technique activates the periaqueductal gray region area of the midbrain, stimulates the noradrenergic descending system and at the level of the spinal cord, the nociceptive afferent barrage is reduced and mechanical hypoalgesia is induced.”
“The clinical importance of the activation of the descending inhibitory pain mechanism should not be ignored since the resulted analgesic effect of this technique can provide a window of opportunity to restore impaired physical performance and disability.”
In April 2019, researchers from Stanford University, the University of Colorado, the University of Sydney, and the University of Illinois College of Medicine, published a study in the official journal of the American Pain Society, the Journal of Pain, titled (26):
Decreased Neurologic Pain Signature Activation
Following Thoracic Spine Manipulation in Healthy Volunteers
These authors used functional magnetic resonance imaging in 10 healthy volunteers to study the effect of spinal manipulation on pain-related activity within brain regions predictive of physical pain. The induced pain was a noxious mechanical stimulation of the right index finger cuticle before and after thoracic spinal manipulation. Functional magnetic imaging was performed with 5 minutes of noxious mechanical stimulation before and after thoracic spinal manipulation.
The index finger cuticle is innervated by the sixth cervical nerve. Hence, any changes in pain perception or pain imaging would not be as a consequence of a thoracic spinal manipulation; if such pain reduction was noted, a plausible explanation would be that the thoracic manipulation activated the descending pain inhibitory control system.
The authors documented a significant decrease in brain pain markers following spinal manipulation. They noted that spinal manipulation’s therapeutic action may be “mediated at the level of the central nervous system.”
In October 2019, the same research group (from reference #26) extended their investigations in patients with neck pain. This study was published in the journal NeuroImage: Clinical, and titled (27):
Evidence for Decreased Neurologic Pain Signature
Activation Following Thoracic Spinal Manipulation
in Healthy Volunteers and Participants with Neck Pain
Once again, these authors used functional magnetic resonance imaging (fMRI) to investigate the effect of thoracic spinal manipulation on pain-related brain activity in 16 subjects with acute/subacute neck pain and compare them to 10 healthy volunteers. The aim of the authors was to extend their investigation to determine if spinal manipulation’s therapeutic action is mediated within the central nervous system. Their primary determination was to document if thoracic spinal manipulation could make meaningful reductions in neck pain.
These investigators found that pain activation decreases following spinal manipulation, and that spinal manipulation alters the processing of pain-related brain activity. They state:
“The findings provide evidence that spinal manipulation may alter pain-related brain activity within brain regions specific to the processing of physical pain, supporting a possible central mechanism of spinal manipulation.”
“A growing body of evidence is pointing towards neurophysiologic mechanisms of action underlying the pain modulating effects of spinal manipulation including both spinal and supraspinal mechanisms.”
“The findings provide evidence that spinal manipulation may alter the processing of pain-related brain activity within specific pain-related brain regions.”
Neck pain and brain pain region activation decreased following thoracic spinal manipulation. These findings were not noted following sham thoracic spinal manipulation. The results suggest a decrease in the nociceptive information reaching supraspinal brain areas.
Most recently (November 2019), an important study on the topic of spinal manipulation activating the brain’s pain descending inhibitory system was published in the Irish Journal of Medical Science, and titled (28):
The Effect of Spinal Manipulation on Brain Neurometabolites
in Chronic Nonspecific Low Back Pain Patients:
A Randomized Clinical Trial
These authors note that in patients with chronic nonspecific low back pain, brain function changes due to the neuroplastic changes. Therefore, the objective of this study was to evaluate the brain metabolite changes after spinal manipulation. They used using proton magnetic resonance spectroscopy for their analysis.
Twenty-five patients with chronic nonspecific low back pain, aged 20–50 years were enrolled in the study. Patients were randomly assigned lumbo-pelvic manipulation or sham.
These patients were evaluated before and 5 weeks after treatment using:
- Numerical Rating Scale
- Oswestry Disability Index
- Proton Magnetic Resonance Spectroscopy
The authors state:
“After treatment, severity of pain and functional disability were significantly reduced in the treatment group vs. sham group.”
The authors also found significant important changes in brain metabolites following low back spinal manipulation that was not found in the sham group. The authors concluded:
“In the patient with low back pain, spinal manipulation affects the central nervous system and changes the brain metabolites. Consequently, pain and functional disability are reduced.”
••••••••••
These studies support the notion that spinal adjusting activates the supra-segmental descending inhibitory pain system. This means that one may not need to adjust the painful spinal segmental level to obtain meaningful pain reduction. Activating this system with narcotic drugs is very problematic. Activating this system through spinal adjusting is plausible and effective for many patients. Recent evidence suggests that chiropractic spinal adjusting for spinal pain syndromes can reduce narcotic use by 64% (29).
REFERENCES
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults: Results From the 2012 National Health Interview Survey; Spine; December 1, 2017; Vol. 42; No. 23; pp. 1810–1816.
- Kuslich S, Ulstrom C, Michael C; The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia; Orthopedic Clinics of North America; Vol. 22; No. 2; April 1991; pp. 181-187.
- Bogduk N; On Cervical Zygapophysial Joint Pain After Whiplash; Spine; December 1, 2011; Vol. 36; No. 25; pp. S194–S199.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine, Second Edition; Lippincott; 1990.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; FA Davis Company; 1996.
- Cailliet R; Low Back Pain Syndrome, 4th edition; F A Davis Company; 1981.
- Parke WW; “Applied Anatomy of the Spine” chapter 2 in Rothman and Simeone; The Spine, second edition; WB Saunders Company; 1982.
- Bland J; Disorders of the Cervical Spine; WB Saunders Company; 1987.
- Bland J; Disorders of the Cervical Spine; Second edition; WB Saunders Company; 1994.
- Offit PA; Pandora’s Lab: Seven Stories of Science Gone Wrong; National Geographic; 2017.
- Bear M, Connors B, Paradiso M; Neuroscience: Exploring the Brain; Second Edition; Lippincott Williams & Wilkins; 2001.
- Jones MR, Viswanath O, Peck J, Kaye AD, Gill JS, Simopoulos TT; A Brief History of the Opioid Epidemic and Strategies for Pain Medicine; Pain Therapy; June 2018; Vol. 7; No. 1; pp. 13-21.
- Irving D; Opioid Rising; Rand Review; Nov/Dec 2015.
- Pert CB, Snyder SH; Opiate receptor: demonstration in nervous tissue; Science; 1973 Mar 9;179(4077); pp. 1011-1014.
- Hosobuchi Y, Adams JE, Linchitz R; Pain relief by electrical stimulation of the central gray matter in humans and its reversal by naloxone; Science; 1977 Jul 8;197(4299); pp. 183-186.
- Restak R; The Brain, The Last Frontier; Warner Books; 1979.
- Kiernan JA: Barr’s The Human Nervous System, An Anatomical Viewpoint; Lippincott-Raven; 1998; pp351-352.
- Nolte J; The Human Brain, An Introduction To Its Functional Anatomy; Mosby; 1999; pp. 270-271; p. 274.
- Kandel E, et.al; Principles of Neural Science; 2000; pp. 482-485.
- Steward O; Functional Neuroscience; Springer; 2000; pp. 218-219.
- Porter J, Jick H; Addiction rare in patients treated with narcotics; New England Journal of Medicine; Jan 10, 1980; Vol. 302; No. 2; p. 123.
- Portenoy RK, Foley KM; Chronic use of opioid analgesics in non-malignant pain: report of 38 cases.; Pain; May 1986; Vol. 25; No. 2; pp.171-86.
- Calabresi M; “They’re the most powerful painkillers ever invented. And they’re creating the worst addiction crisis America has ever seen”; Time;
June 15, 2015. - Vicenzino B, Collins D, Wright A; The Initial Effects of a Cervical Spine Manipulative Physiotherapy Treatment on the Pain and Dysfunction of Lateral Epicondylalgia; Pain; November 1996; Vol. 68; No. 1; pp. 69-74.
- Savva C, Giakas G, Efstathiou M; The role of the descending inhibitory pain mechanism in musculoskeletal pain following high-velocity, low amplitude thrust manipulation: a review of the literature; Journal of Back Musculoskeletal Rehabilitation; 2014; Vol. 27; No. 4; pp. 377-382.
- Weber K, Wager T, Elliott J, Mackey S, Liu W, Sparks C; Decreased Neurologic Pain Signature Activation Following Thoracic Spine Manipulation in Healthy Volunteers; The Journal of Pain; April 2019; Vol. 20; No. 4; Supplement; p. S69.
- Weber K, Wager T, Elliott J, Mackey S, Liu W, Sparks C; Evidence for Decreased Neurologic Pain Signature Activation Following Thoracic Spinal Manipulation in Healthy Volunteers and Participants with Neck Pain; NeuroImage: Clinical; October 18, 2019; Vol. 24; 102042.
- Didehdar D, Kamali F, Yoosefinejad AK, Lotfi M; The effect of spinal manipulation on brain neurometabolites in chronic nonspecific low back pain patients: a randomized clinical trial; Irish Journal of Medical Science; November 2019; [epub].
- Corcoran KL, DC, Bastian LA, Gunderson CG, Steffens C, Brackett MA, Lisi AJ; Association Between Chiropractic Use and Opioid Receipt Among Patients with Spinal Pain: A Systematic Review and Meta-analysis; Pain Medicine; September 2019; [epub].
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”